Rectal bleeding can be an alarming symptom, often signaling underlying issues like hemorrhoids, anal fissures, inflammation, or even cancer.
As a colon hydrotherapist with years of experience, I’ve seen firsthand how cultural sensitivities prevent many from discussing or understanding their anal health. Yet, the anus is a highly sensitive area, and changes like itching, pain, or visible blood on the stool—medically termed hematochezia—demand attention. In this article, I’ll explore the causes of rectal bleeding, its symptoms, and practical steps to address and prevent it, drawing on my expertise to guide you toward better digestive wellness.
Why Rectal Bleeding Happens
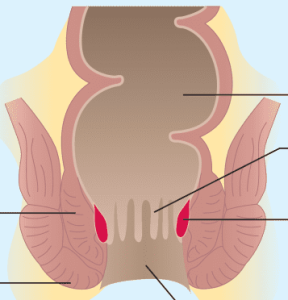
Rectal bleeding is a symptom I encounter frequently in my practice, and it’s often tied to common conditions. Hemorrhoids, affecting nearly 70% of adults in Western countries at some point, especially between ages 45 and 65, top the list. These swollen veins in the anal canal can cause bright red blood on toilet paper or stool, along with itching and swelling. Anal fissures—small tears in the anal lining—are another frequent culprit, bringing sharp pain and similar bleeding. Both are widespread, yet manageable with proper care.
More serious causes include anal prolapse, rectal prolapse, anal vein thrombosis (often misnamed “external hemorrhoids”), fistulas, abscesses, or even anal rim cancer. In the large intestine and rectum, conditions like diverticula (pouches in the intestinal wall), polyps, inflammation (e.g., proctitis), or colon cancer can also trigger bleeding. Even rarer issues, like vascular malformations or endometriosis affecting the bowel, may be at play. With age, the risk of these pathologies rises, sometimes worsened by medications like blood thinners.
Symptoms to Watch For
Beyond rectal bleeding, other red flags include changes in bowel habits, abdominal pain, bloating, fatigue, or unexplained weight loss. These could point to deeper gastrointestinal issues needing urgent medical review. In my work, I’ve noticed clients often delay seeking help due to embarrassment, but early action is critical—especially when blood is persistent or paired with these symptoms.
Diagnosis and Treatment
When rectal bleeding occurs, a doctor will first assess your medical history—think anticoagulant use or signs of bleeding tendencies (e.g., frequent bruising or nosebleeds). Procedures like colonoscopy allow direct inspection of the colon and rectum, enabling tissue sampling or polyp removal to prevent cancer. In my practice, I’ve seen how these interventions, paired with tailored diets (low-lactose or gluten-free, if needed), can transform gut health. Prompt diagnosis is key—some causes require urgent care, while others benefit from lifestyle adjustments.
Preventing Rectal Bleeding Naturally
A healthy bowel is your best defense against rectal bleeding and related issues. A high-fiber diet with five daily servings of fruits and vegetables promotes regular bowel movements, reducing strain that worsens hemorrhoids or fissures. Pair this with 30–60 minutes of daily exercise, minimal alcohol and smoking, and a low-fat, low-sugar diet to support blood vessel health. Good hygiene and breathable clothing further protect the anal area.
Conclusion
Rectal bleeding, whether from hemorrhoids or something more serious, isn’t a topic to shy away from. With my background in colon hydrotherapy, I urge you to overcome any hesitation and seek answers. Combining medical insight with proactive habits can keep your digestive system thriving. If you’re noticing symptoms, consult a healthcare provider—your peace of mind and health are worth it.




0 Comments